The evolution of glucagon: From emergency glucagon kits and pre-filled syringes to nasal sprays and autoinjectors
Learn about three major advances in treating severe low blood sugar (severe hypoglycemia)
The risk of severe low blood sugar can feel overwhelming for anyone with diabetes using insulin or other diabetes medications known to cause low blood sugar. Also known as severe hypoglycemia, these lows occur when blood sugar drops below a certain level, causing physical and mental changes that can include headache, fatigue, seizures and even loss of consciousness. While hypoglycemia can be treated by eating sugar or a sugar-sweetened product, a severe low requires faster medical treatment — typically with a glucagon injection.
It’s important for diabetes patients, their caretakers and the individuals involved in their day-to-day life to know the signs of severe hypoglycemia — so it can be quickly treated. A medication called glucagon is a potentially life-saving tool for correcting these severe lows.
Who is at risk of a severe low?
For patients with diabetes, those with type 1 diabetes are three times as likely to experience hypoglycemia than those with type 2 diabetes. You may be at risk of a severe low if you:
- Take insulin or sulfonylureas
- Exercise at an intense level
- Tend to skip meals
- Have an inconsistent schedule
- Feel stressed most of the time
- Have tight blood sugar goals
- Have insulin pump problems
- Are more sensitive to insulin
Glucagon’s role in raising blood glucose levels
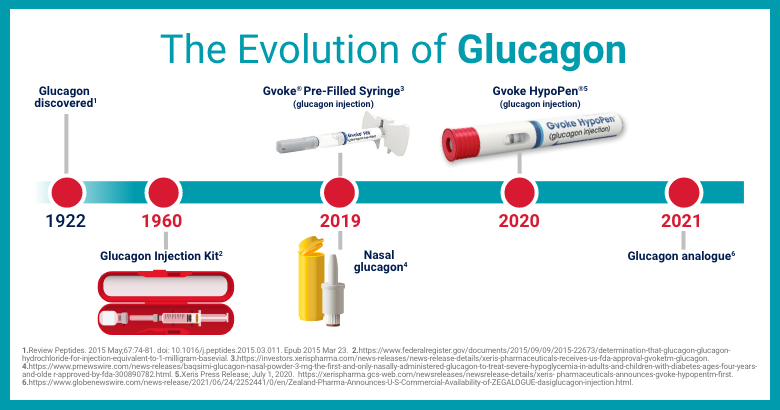
Glucagon is a hormone that plays a critical role in quickly raising the body’s blood sugar levels to restore balance. It was discovered and studied since 1922. Over time, there have been three major advances in the administration of glucagon for treating severe lows:
1. Emergency glucagon kit
The first glucagon kit became available in 1960. These life-saving kits contain a vial of glucagon powder and a syringe filled with saline. They require preparation time and someone to administer the injection using the syringe. Eli Lilly and Novo Nordisk are two of the largest suppliers of these glucagon emergency kits, although Lilly recently announced that its kit will be discontinued by the end of 2022.
2. Prefilled syringe and nasal spray
As the science behind glucagon injections continued to advance, it became clear that giving diabetes patients and their caregivers an easier, faster way to administer glucagon was necessary. In 2019, pre-filled glucagon syringes became available for adults and children, as well as a needleless nasal spray, which doesn’t require inhalation.
3. Glucagon autoinjector
The most recent advancement in administration of glucagon comes in the form of an autoinjector. Gvoke HypoPen® (glucagon injection) is the first premixed glucagon autoinjector used to treat very low blood sugar in adults and children ages 2 years and above with diabetes. It can be administered in two simple steps, pull red and push yellow.1,2 In 2021, the first glucagon analog autoinjector was released. Glucagon autoinjectors typically have a simpler administration process than emergency glucagon kits — they don’t require mixing and have no visible needles.
From glucagon kits to ready-to-use options, innovation in the treatment of severe lows has made it easier for diabetes patients and their caregivers to manage type 1 diabetes and type 2 diabetes. No matter which glucagon option you choose, the most important thing to remember is to always be prepared — so you can focus more on the people, places and activities that bring you joy.
REFERENCES:
- Gvoke HypoPen [instructions for use]. Chicago, IL: Xeris Pharmaceuticals, Inc.
- Valentine V, Newswanger B, Prestrelski S, Andre AD, Garibaldi M. Human factors usability and validation studies of a glucagon autoinjector in a simulated severe hypoglycemia rescue situation. Diabetes Technol Ther. 2019;21(9):522-530
US-GVK-22-00067(v4) 9/25
Indication
GVOKE (glucagon) is a prescription medicine used to treat very low blood sugar in adults and children ages 2 years and above with diabetes.
Important Safety Information
- Do not use GVOKE if you:
-
- Have a tumor in the gland on top of your kidneys, called a pheochromocytoma because of the risk of a substantial increase in blood pressure
- Have a tumor in your pancreas called an insulinoma because of the risk of low blood sugar
- Are allergic to glucagon or any inactive ingredient in GVOKE. Stop using GVOKE and seek immediate medical attention if you experience any symptoms of a serious allergic reaction such as rash, difficulty breathing, or low blood pressure
- Before using GVOKE, tell your doctor about all the medicines you take and your medical conditions, including if you have not had food or water for a long time (prolonged fasting or starvation), have low blood sugar that does not go away (chronic hypoglycemia), or have a history of a skin rash called necrolytic migratory erythema (commonly associated with glucagon-producing tumors)
- The most common side effects reported in adults are nausea, vomiting, swelling at the injection site, and headache
- The most common side effects reported in children are nausea, low blood sugar, vomiting, headache, abdominal pain, high blood sugar, pain or redness at injection site, and hives
- Inform caregivers on the Instructions for Use of GVOKE, and symptoms of severe hypoglycemia, which include unconsciousness and seizures or convulsions
- Store in original container until time of use, and at room temperature between 68°F to 77°F (20° C to 25° C)
- You are encouraged to report side effects of prescription drugs to the FDA. Visit http://www.fda.gov/medwatch or call 1-800-FDA-1088
Please talk to your doctor and see full Prescribing Information and Patient Information Guide for GVOKE.