There’s a lot of planning and stress involved in going back to school – whether it’s your child’s first year of preschool or they’re returning to school after a type 1 diabetes diagnosis. From wondering what to discuss with your child’s teachers to trusting they’ll be taken care of if they experience a low, there is so much to think about.
We spent the last few months preparing for Emma to walk through her school doors this fall. It’s the first time her diabetes care will be in someone else’s hands. So, if you’re anxious (like we are!) about the big day ahead, here are our suggestions – including our favorite glucagon rescue pen and hypoglycemic snacks – to conquer any grade level with type 1 diabetes.
Get to know your school nurse.
Like any relationship, communication is key! And the relationship between you, your child and their school nurse is no different. Here’s how to establish a good relationship:
- Meet with the school nurse before school starts to introduce your child and relieve any anxieties.
- Establish a plan for daily contact.
- If your child is on a Dexcom® continuous glucose monitor, make sure to send the nurse an invite to follow your child on the Dexcom® Follow app.
- Review your doctor’s supply orders with the nurse. These orders provide guidelines for treating lows and correcting high blood sugar. (We’ll share more info in another post about supply orders and 504 plans.)
- Ensure anyone involved in your child’s care can recognize symptoms of low blood sugar and knows what to do in an emergency to keep your child safe.
More tips from a school nurse
Emma’s nana, Lori Trites, BSN, RN, NCSN, has been a school nurse for 20 years. She’s cared for many students with type 1 diabetes in all age groups and with a wide variety of diabetes technology — and she shared a few of her insights with us:
- Ensure your school’s health office has necessary supplies – including extra insulin and needles, fully stocked glucometer kit, ketone test kit, quick-acting glucose snacks for lows, extra water for highs and extra pump supplies.
- Make sure the nurse has Gvoke HypoPen® (glucagon injection) on hand. It’s a preferred choice because it can be administered in just two steps.
- Create a “lockdown kit” for each classroom in case of emergency with important phone numbers (parents and doctors), extra testing kit, juice boxes, fast-acting low snacks and glucagon.
Prepping supplies.
Research, research, research! There are many treatment supplies available for your child’s diabetes. Make sure you review them and speak with your doctor about what’s best for your child. I’ve broken the supplies into three categories: insulin delivery, blood sugar monitoring and emergency glucagon. Each of these categories requires training the school staff and a little preparation from you.
Insulin delivery
We all know there are three main ways to deliver insulin: pump, pen and syringe. If your child is old enough, talk with them to see if they’re comfortable with their current insulin intake method. Emma is on Omnipod® 5 – and based on her reaction when we give her shots, she’s comfortable with it. If your child is interested in switching from one method of insulin delivery to another, ask your doctor if it’s worth making a change before school starts.
When you’ve chosen an insulin delivery method for school, meet with the school nurse to make sure they have the necessary training. If your child is used to a certain way of administering the insulin, share that with the nurse, too. For example, do you ice the injection site first? Do you sing a song or hold their hand? Creating a consistent delivery method will help your child feel comfortable and safe.
Blood sugar monitoring
If your insurance covers the cost of a CGM, I highly suggest getting one. Emma uses Dexcom® G6, which lets me and her nurse monitor her sugar while she’s in the classroom. We can set alerts to indicate when it’s below or above a certain number. Select models of the Freestyle Libre® monitor have similar apps that let you monitor blood sugar when you’re away from your child.
If a CGM is not an option, set up a plan with the nurse as to how often they’ll check your child’s blood sugar. This should also be outlined in your doctor’s school orders. Make sure to restock test strips and lancets regularly!
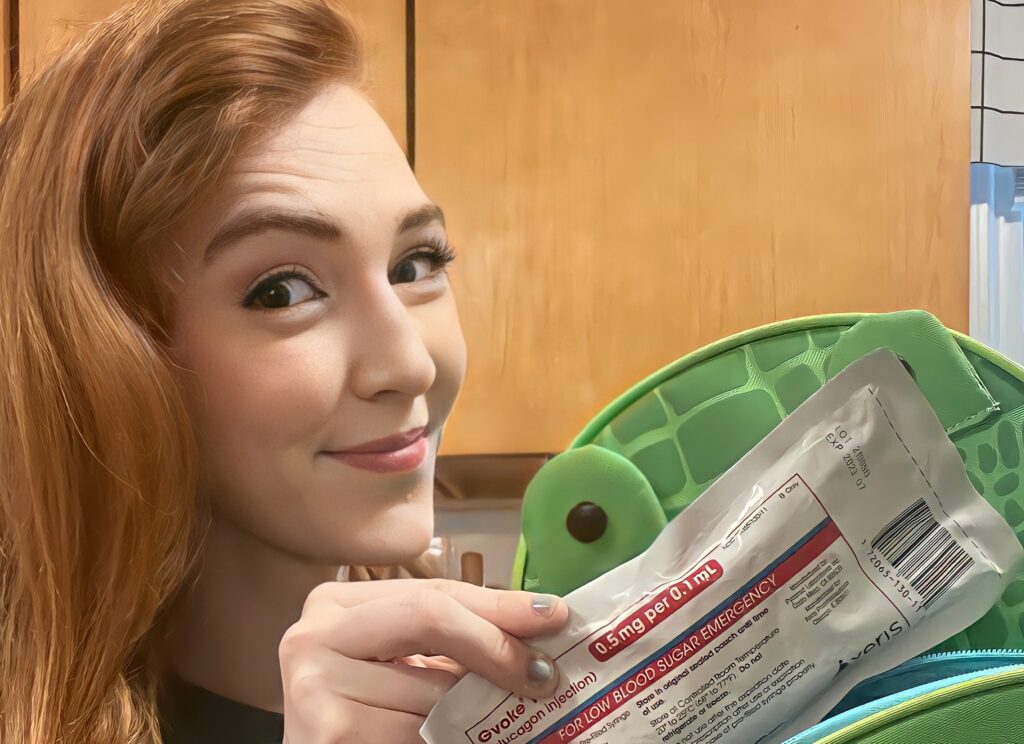
Emergency glucagon
Glucagon is a prescription medication for very low blood sugar, and there are a few options to choose from. We chose Gvoke HypoPen® for Emma. It’s a premixed autoinjector that’s ready to use to treat very low blood sugar in adults and kids with diabetes ages 2 and above. It can be administered by anyone in two steps: pull the red and push the yellow. But Gvoke®isn’t for everyone. Just like any prescription, it’s important to understand safety information. For example, you should not use Gvoke® if you have certain tumors in your adrenal glands and pancreas because it can cause severe high blood pressure or low blood sugar. And, you shouldn’t use it if you are allergic to any of the ingredients because allergic reactions can be severe.
Unlike many options, Gvoke HypoPen® is a glucagon injection that does not have a visible needle, making the process less scary. It’s available for both children and adults (0.5MG/0.1ML kid’s dose and 1 MG/0.2ML adult dose). It can be used to treat a severe low if:
- Correcting with food or drink isn’t working
- Your child can’t swallow safely
- Your child feels like passing out
- Your child is unresponsive or seizing
Make sure the school nurse, teacher and any other adult who cares for your child is trained on how to administer glucagon. There are instructions right on the package insert. You can also find helpful resources on its website, including how-to videos and FAQs.
Remember to supply your child with their favorite hypoglycemic snacks, too. A few great options for “hypo snacks” include juice, glucose tabs, frosting, fruit snacks and smarties. Emma’s favorite is fruit snacks!
More supply management tips:
- Make a list of all the supplies you pack and note each item’s expiration date so you can check to see when replacements are needed.
- Pack a list of emergency phone numbers in both the nurse’s kit and classroom kits. That way, a substitute nurse or teacher knows who to contact if they need to supply care.
- In the classroom kits, write general instructions on how to treat a low and administer insulin in case of emergency lockdown.
- Use a small tackle box for the nurse’s supplies. That way, each supply will have its own compartment and you’ll be able to tell when it needs to be restocked.
- Small transparent makeup bags are great to use for a lockdown emergency kit for each classroom.
- It can get expensive to stock up on diabetes supplies, so look for financial assistance and coupons.
- Set up a communication plan with the nurse to alert you when supplies are running low (when you have about a week left), so you’ll have enough time to pick up prescriptions and get them to school.
- Make sure your child’s pick-up list is up to date. If you work and can’t get away to help with an unexpected pump change-out or sickness, assign trustworthy people who may be able to pick up your child and assist until you get home.
Helping your child prepare and adjust.
No matter your child’s age, it can be scary for them to transition from a parent to a nurse caring for their diabetes. Here are a few tips to ease the transition:
Familiar faces
Have your child join you when you meet the school nurse so they can get familiar with both the nurse and their office.
Social story
Through Emma’s experience with diabetes, we’ve learned that social stories can be an amazing tool for preparing any child for a new situation. Social stories use photos to help a child understand what they can expect from a new situation. You can create one about a day at school and one about diabetic care at school.
Imaginary school
Before school starts, do a day of play school. Have your child sit at a table and pretend you’re the teacher. Give them a few fun worksheets. Tell them when they should sit for story time and have them come to you before lunch for insulin from the nurse’s office. This will help them understand the flow of a school day.
I get it – it’s tough to trust other people with your precious child’s diabetes care. But making sure everyone is as prepared as possible will help the transition go smoothly for both you and your child. Good luck! I’m sending you all the love and strength you need for a successful first day.
Gvoke® is a prescription medicine used to treat very low blood sugar (severe hypoglycemia) in adults and kids with diabetes ages 2 year and above. It is not known if Gvoke® is safe and effective in children under 2 years of age.
Do not use Gvoke® if you have a tumor in the gland on top of your kidneys (adrenal gland), called a pheochromocytoma; you have a tumor in your pancreas, called either insulinoma or glucagonoma; you are allergic to glucagon or any other inactive ingredient in Gvoke®.
Gvoke® may cause serious side effects, including high blood pressure: Gvoke® can cause high blood pressure in certain people with tumors in their adrenal glands. Low blood sugar: Gvoke® can cause low blood sugar in certain people with tumors in their pancreas. Serious skin rash: Gvoke® can cause a serious skin rash in certain people with a tumor in their pancreas called glucagonoma. Serious allergic reaction: Call your doctor or get medical help right away if you have a serious allergic reaction including rash, difficulty breathing, low blood pressure.